Cracking the Interoperability Code: How to Build a Truly Connected Health System in India

India’s healthcare data is growing at a scale never seen before, reflecting both the digitization wave and the rising burden of care. In 2020 alone, global healthcare data touched 2,314 exabytes. Yet, much of this data sits in unconnected silos, limiting its value in real-time clinical decisions and long-term population health planning.
Interoperability, the ability of different health systems to exchange and use information seamlessly, is no longer optional. It is the foundation for delivering coordinated, patient-centric care across hospitals, diagnostic centers, insurers, and government health registries.
But for India, true interoperability remains a complex challenge. It is not just about moving data, but about preserving its structure, context, and accuracy as it travels across platforms. This requires both technical alignment and strong governance.
In this article, we break down how leading countries like the UK, US, and others approached the interoperability puzzle and what India must priorities to build a digitally connected health system.
India’s Interoperability Efforts: A Mixed Picture
The volume of health data is expanding at a staggering pace, with global digital health information projected to grow at 48% annually through 2025. This surge has spurred major investments in data infrastructure and interoperability tools, with healthcare systems worldwide spending close to $18.6 billion each year on digital transformation.
One influential study by researcher Sriram Sitaraman, published in the International Journal of Computer Engineering and Technology, outlines how this data wave is reshaping clinical delivery. It points to meaningful progress in dismantling silos, building interoperable systems, and aligning digital strategies across care settings.
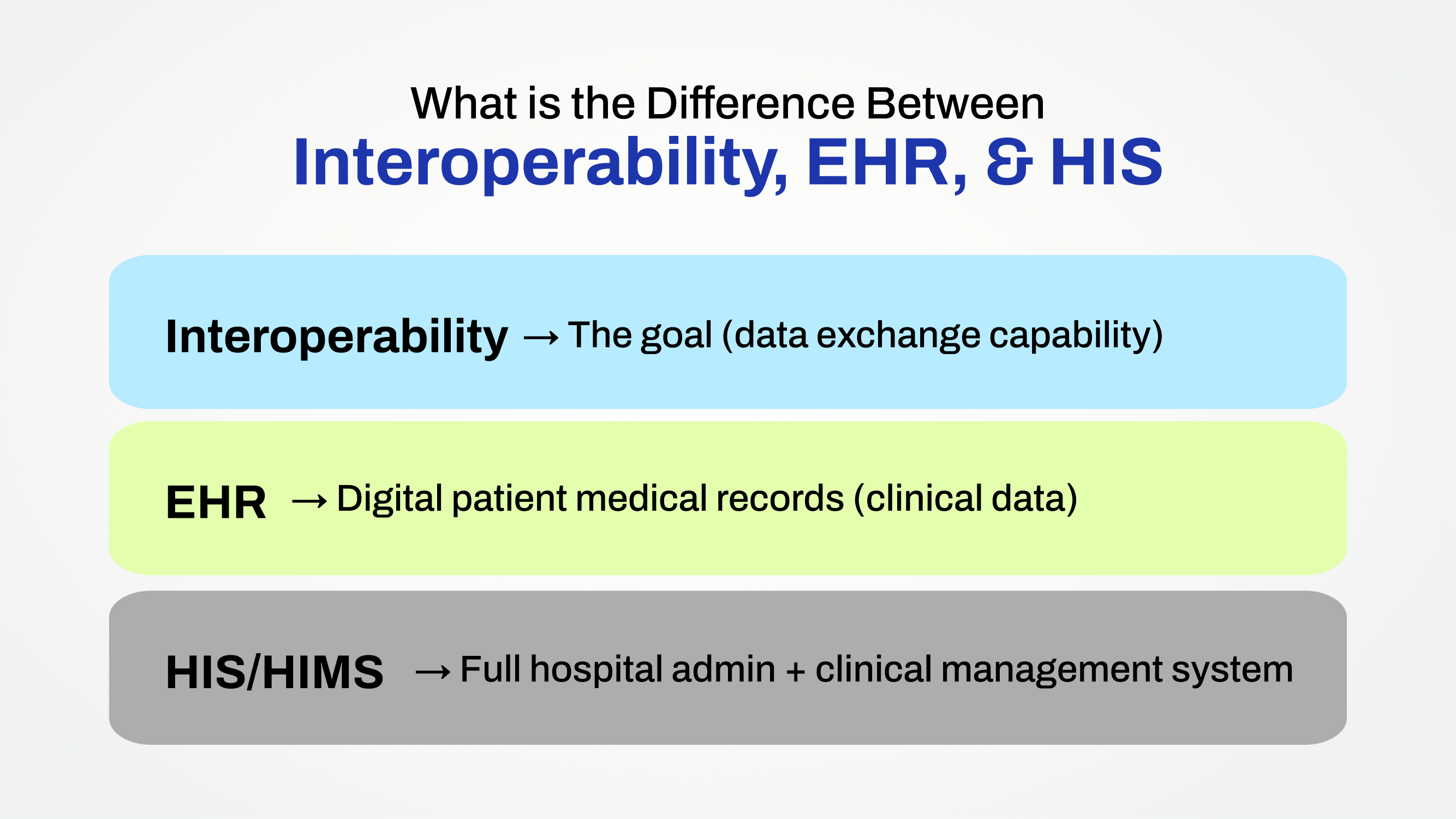
While interoperability is gaining traction, it’s often misunderstood or conflated with electronic health records (EHRs) and hospital information systems (HIS). Before we dive deeper, the table below draws clear distinctions between these terms, closely related but functionally distinct pillars of digital health.
India’s Healthcare Data Is Growing, But Can We Use It?
India has made strong moves toward healthcare digitization, but interoperability remains uneven. Flagship efforts like the Ayushman Bharat Digital Mission (ABDM) have created vital infrastructure, yet true, seamless data exchange across hospitals, labs, insurers, and government systems is still the exception rather than the norm.
By early 2025, the National Health Authority reported over 3.49 lakh facilities registered in ABDM’s Health Facility Registry. However, only around 12% are fully connected to the Health Information Exchange, which enables real-time, standardized data sharing. Meanwhile, just 35% of Indian hospitals use electronic medical records, mostly in urban and private networks.
Fragmentation remains a core challenge. Public and rural health facilities still rely heavily on paper-based or isolated digital systems, making integrated care difficult. Unless these gaps are bridged, India risks digitizing in silos, losing out on the full potential of a connected health system.
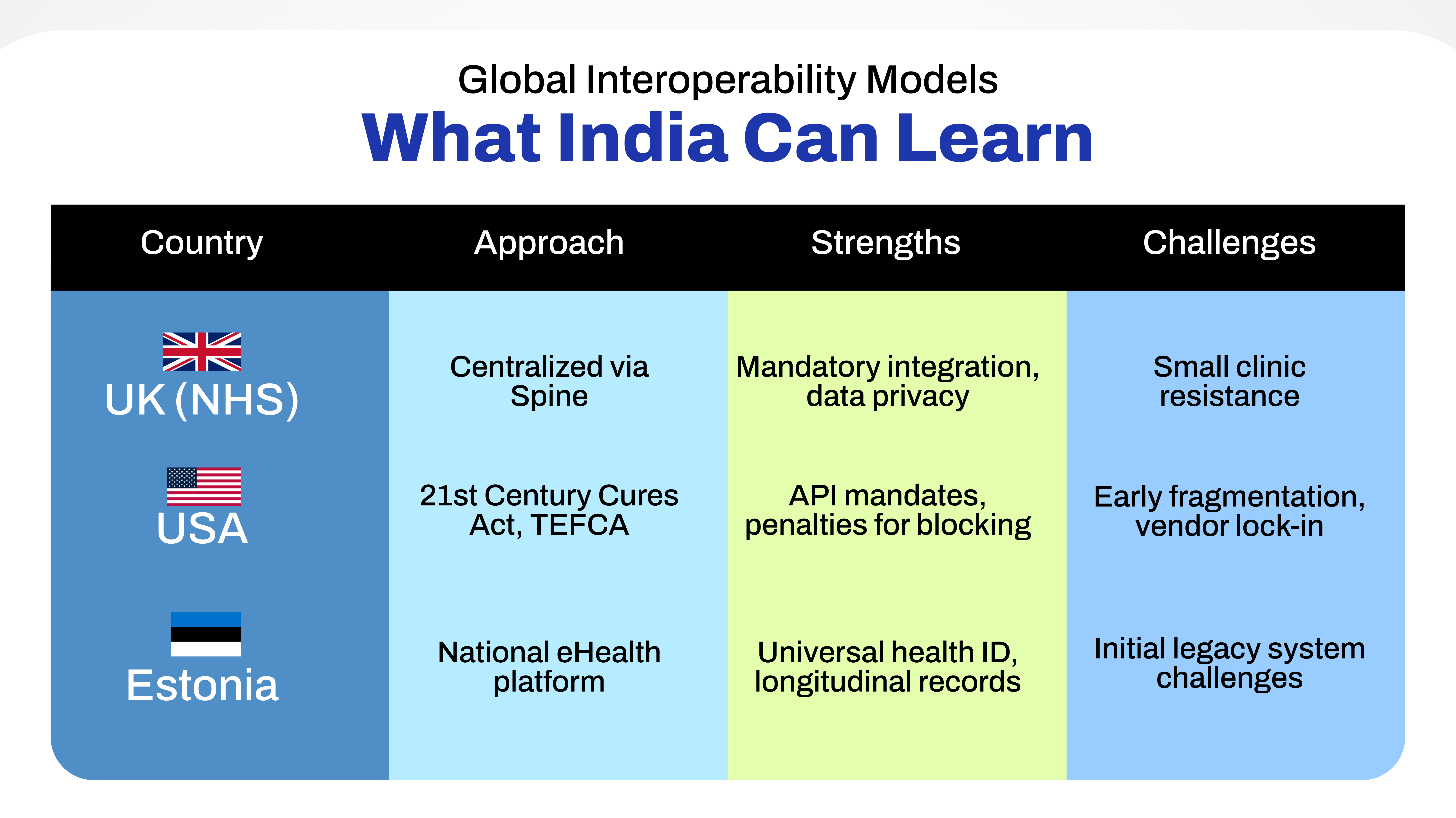
Global Interoperability Models: What India Can Learn
India’s digital health push is at a pivotal point. The building blocks, health IDs, national registries, sandbox APIs, are in place. But if we’re serious about creating a connected, patient-first ecosystem, we must learn from systems that have been through this grind. Countries like the UK, US, and Estonia offer not perfect templates, but useful insights, especially on the "how" behind interoperable health systems, how they got providers on board, governed standards, funded transitions, and enforced accountability.
United Kingdom (Centralized backbone, slow adoption curve)
The UK’s NHS was one of the first to try national-scale interoperability. Its core infra, a central system called Spine, connects GPs, hospitals, emergency services, and pharmacies. Every citizen has a unique health number, and providers are expected to plug into this network.
But while the design was sound, implementation faced friction. Older hospital IT systems, resource constraints, and inconsistent API adoption meant full-scale interoperability is still patchy. The UK's experience reminds us that having a national backbone isn’t enough. You need sustained, on-ground tech support and upgrade funding for diverse providers, especially in Tier 2 and rural areas.
United States (Regulation-driven, market-led approach)
Unlike the UK, the US didn't build one system, it enforced rules. With multiple private EMRs in play, the government used laws like the 21st Century Cures Act to mandate open APIs, penalize data blocking, and give patients legal rights to their records.
It’s not seamless yet, but it shifted the industry. Hospitals and EMR vendors had to comply, and now TEFCA is creating a national health data exchange framework. For India, the US example shows the value of legislative teeth, especially when dealing with large private hospital chains or platform players reluctant to share data.
Estonia (Digital-first, small but mighty)
Estonia may be tiny, but it built one of the world’s most integrated health data systems. Every citizen has a digital ID, and all healthcare interactions, clinic visits, test results, prescriptions, get logged in a single system accessible across the network. It worked because of early digital governance, phased onboarding, and government grants that helped even small clinics modernize. The key message here? Size isn’t the only factor. What matters is a long-term plan, strict adherence to national standards, and state support for digital capacity-building.
For India, these examples offer a common takeaway: interoperability is not solely a technical exercise but a governance, incentive, and trust-building challenge. Mandatory compliance frameworks, patient data rights, financial incentives for smaller hospitals, and public-private coordination are as crucial as API protocols and health data standards. India’s Ayushman Bharat Digital Mission will need to adapt these learnings to its highly decentralized, state-driven, and mixed public-private healthcare ecosystem if it hopes to scale interoperability beyond urban corporate hospitals.
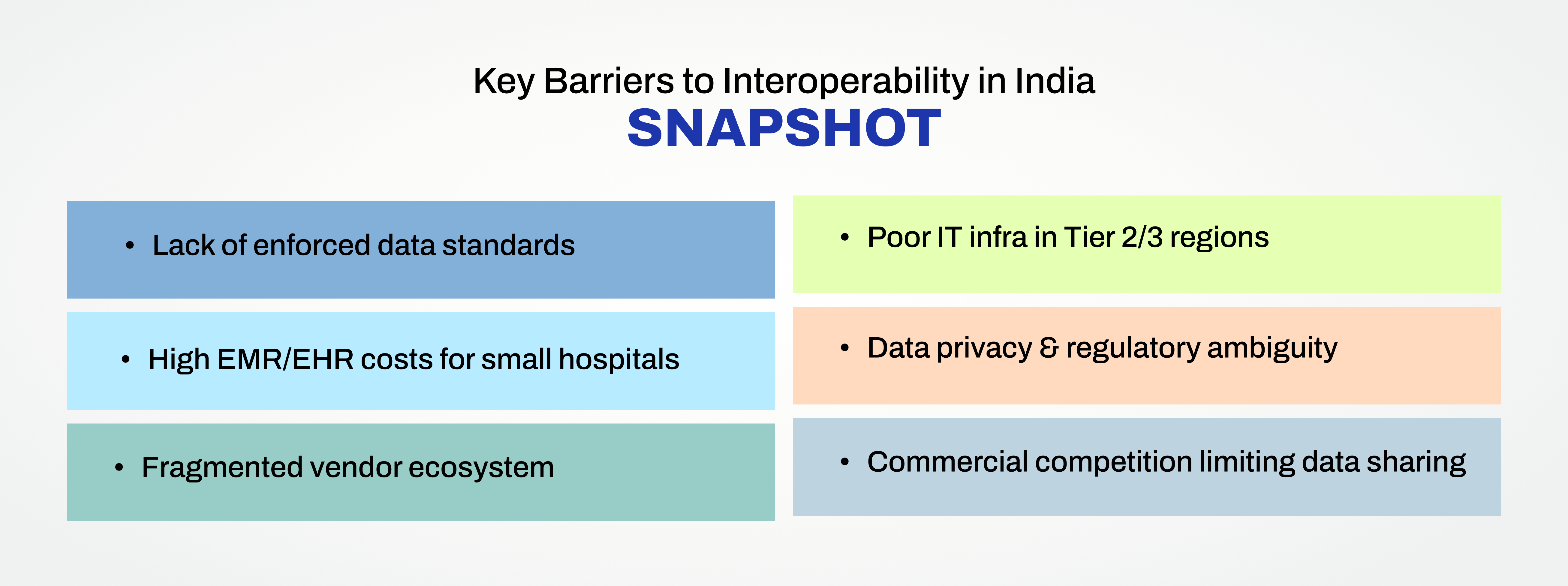
What’s Blocking Interoperability in India?
Despite steady progress in digital health adoption, India faces several entrenched barriers that hinder true interoperability. These challenges are structural, technical, financial, and regulatory, and without addressing them systemically, nationwide health data exchange will remain limited to isolated success stories.
The absence of universally enforced data standards is one of the most pressing issues. While the Ayushman Bharat Digital Mission recommends adopting FHIR (Fast Healthcare Interoperability Resources) and SNOMED CT standards, compliance remains voluntary for private providers. As a result, many hospitals continue to use proprietary EMR systems that do not natively support data exchange outside their own networks.
Cost remains a significant deterrent for small and mid-size hospitals, particularly in Tier 2 and Tier 3 cities. Comprehensive EMR and interoperability solutions require not just software investment but also upgrades in hardware, networking infrastructure, and skilled IT support, all of which stretch the budgets of smaller healthcare facilities already under operational strain.
India’s fragmented vendor ecosystem further complicates the issue. Hundreds of hospital software providers operate in silos, with little incentive to build open, interoperable systems. Many EMR vendors have built proprietary platforms optimized for internal use but incapable of communicating with ABDM’s Health Information Exchange or with other hospital systems. This competitive, disconnected software market reinforces data silos and undermines integration efforts.
Infrastructure gaps in non-metro regions are another major hurdle. Many government hospitals, standalone clinics, and rural health centers still lack reliable internet connectivity, secure data storage systems, and basic digital infrastructure, prerequisites for participating in a real-time, nationwide health data network.
Data privacy concerns and regulatory uncertainty also fuel reluctance, especially among private hospitals and diagnostic labs. While India’s forthcoming Digital Personal Data Protection (DPDP) Act aims to bring clarity, ambiguity around data ownership, consent frameworks, and health data classification continues to delay integration initiatives.
A cultural reluctance to share data due to commercial competition between private hospitals and between public and private providers compounds the problem. For many organizations, health data remains a commercial asset rather than a shared public good, limiting the collective willingness to participate in interoperable networks.
At the heart of these challenges lies a difficult but unavoidable question is India’s healthtech market incentivized enough for interoperability, or does data ownership continue to function as competitive leverage? Until this tension is resolved, through policy mandates, aligned incentives, and shared governance, true interoperability will remain elusive.
Key Barriers to Interoperability in India
ABDM’s Interoperability Journey: Progress & Pending Gaps
The Ayushman Bharat Digital Mission (ABDM) is India’s most ambitious initiative to unify its fragmented health data systems. Designed to enable federated and interoperable health information exchange, the mission aims to provide every citizen with a unique Ayushman Bharat Health Account (ABHA), register all healthcare facilities in a national Health Facility Registry (HFR), and support seamless digital record sharing through the Health Information Exchange and Consent Manager (HIE-CM) platform.
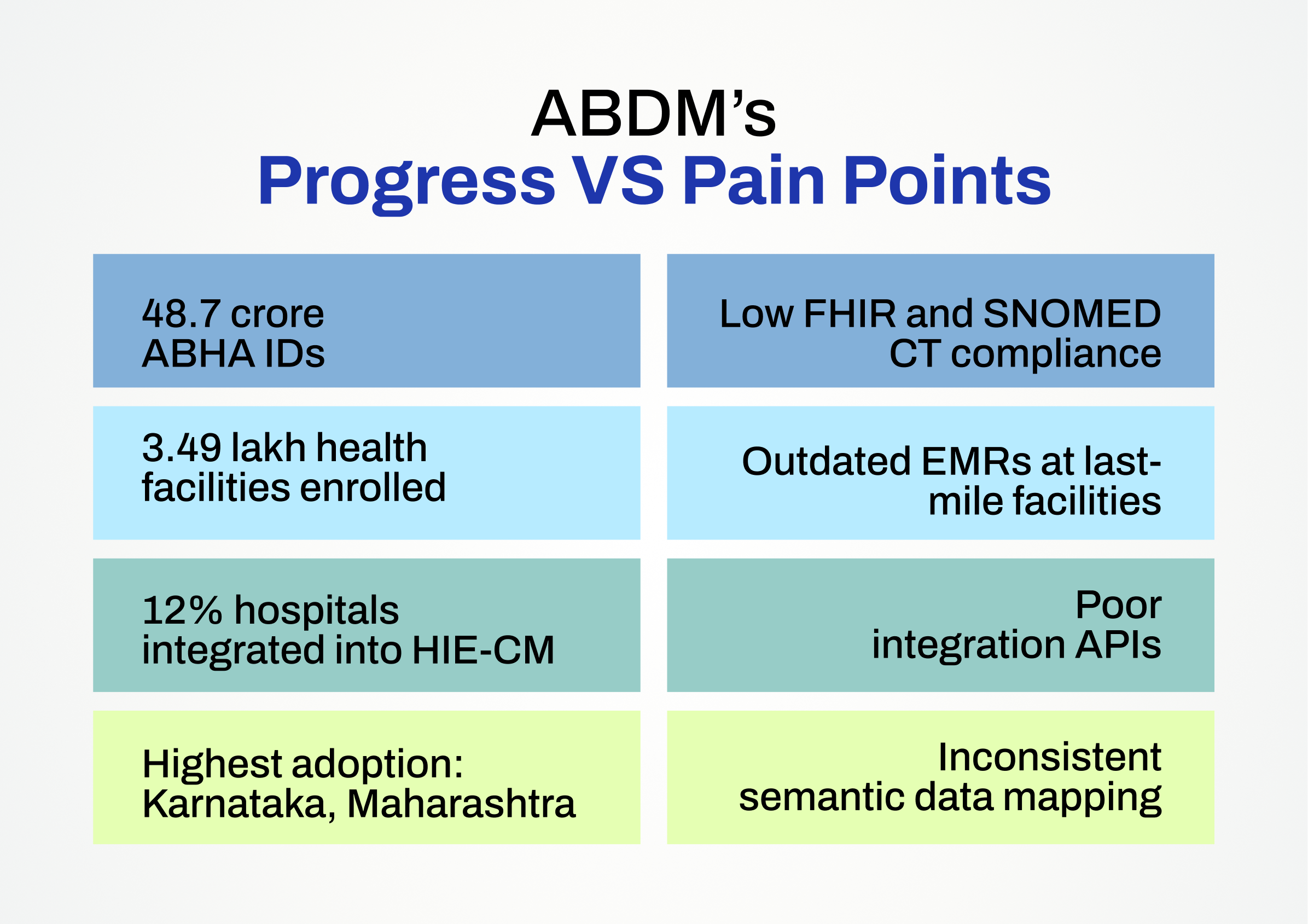
The scale of the rollout has been impressive. By February 2025, over 3.49 lakh health facilities were registered on the HFR and more than 48.7 crore ABHA IDs had been generated. This establishes a solid foundation for a nationwide digital health ecosystem.
However, integration remains uneven across the country. Only about 12 percent of facilities have achieved full interoperability with the HIE-CM platform. Most integrated hospitals are large private chains or tertiary government centers in digitally advanced states like Karnataka and Maharashtra. In contrast, smaller clinics, standalone hospitals, and district-level government facilities continue to operate on outdated systems that are not linked to ABDM.
Technology gaps are a major barrier. Many providers still use older EMR software that does not support ABDM’s APIs. Limited use of clinical standards such as SNOMED CT and partial implementation of FHIR-based data formats result in incomplete or inconsistent record sharing. Lab results, discharge summaries, and imaging data often fail to transfer in structured formats.
Legacy systems, closed-loop EMRs, and poor data mapping further restrict interoperability. Integration readiness assessments by the National Health Authority and state governments consistently flag these as key challenges, particularly in Tier 2 and Tier 3 facilities.
Although ABDM’s federated model preserves patient data ownership at the source, the lack of clear responsibility for data quality and semantic consistency has caused frequent breakdowns in real-time data exchange.
For ABDM to succeed, infrastructure alone is not enough. Closing the gaps in governance, enforcing standards, and creating stronger incentives for hospitals to participate will be critical. Without these, India risks digitizing its healthcare system without truly connecting it.
Building a Connected Health Ecosystem: What Needs to Happen
India’s digital health infrastructure is steadily expanding, but achieving nationwide interoperability will require more than piecemeal integrations. It demands a coordinated effort to align technical standards, financial incentives, regulatory frameworks, and public-private partnerships. Several critical steps can help close the existing gaps and build a truly connected healthcare ecosystem.
The most immediate priority is enforcing the adoption of globally recognized interoperability standards, particularly FHIR (Fast Healthcare Interoperability Resources) and SNOMED CT for clinical terminologies. While ABDM recommends these, making them mandatory for all EMR/EHR tenders, integrations, and private health IT solutions will ensure consistency in how health data is captured, structured, and exchanged.
For small and mid-sized hospitals, especially in Tier 2 and 3 cities, financial incentives and subsidized digital health programs are essential. The high capital and operational costs of implementing EMR systems and interoperability solutions have kept many facilities offline or reliant on basic software without integration capabilities. Direct government subsidies, soft loans, and integration grants could accelerate digital adoption in these settings.
Interoperability mandates should be built into every new EMR/EHR procurement tender, whether in the public or private sector. Health systems must be obligated to procure only those digital solutions that support open APIs, standardized data exchange protocols, and ABDM’s HIE-CM integration. Without regulatory compulsion, proprietary and closed systems will continue to thrive.
Strengthening India’s health data protection laws is another foundational requirement. The Digital Personal Data Protection (DPDP) Act, expected to come into effect in 2025, offers a crucial opportunity to align data privacy regulations with interoperability goals. Clear guidelines on consent management, data security, audit protocols, and patient rights over their digital health records will build the trust necessary for voluntary data sharing between providers.
Private sector participation will be vital in scaling interoperability. Beyond hospitals and clinics, medtech firms, diagnostics labs, insurers, teleconsultation platforms, and health apps must be integrated into ABDM’s data exchange networks. Making interoperability compliance a prerequisite for licensing or market access in these sectors could be a powerful policy lever.
Ultimately, achieving true interoperability in India is not a technical challenge alone. It is a governance issue, an incentive alignment challenge, and a trust-building exercise.
To better understand where India truly stands on the path to digital interoperability, the snapshot below captures key national indicators, from ABHA adoption and EMR penetration to HIE-CM integration and FHIR uptake. While progress is undeniable, the data highlights how much work remains to achieve a truly connected health ecosystem.
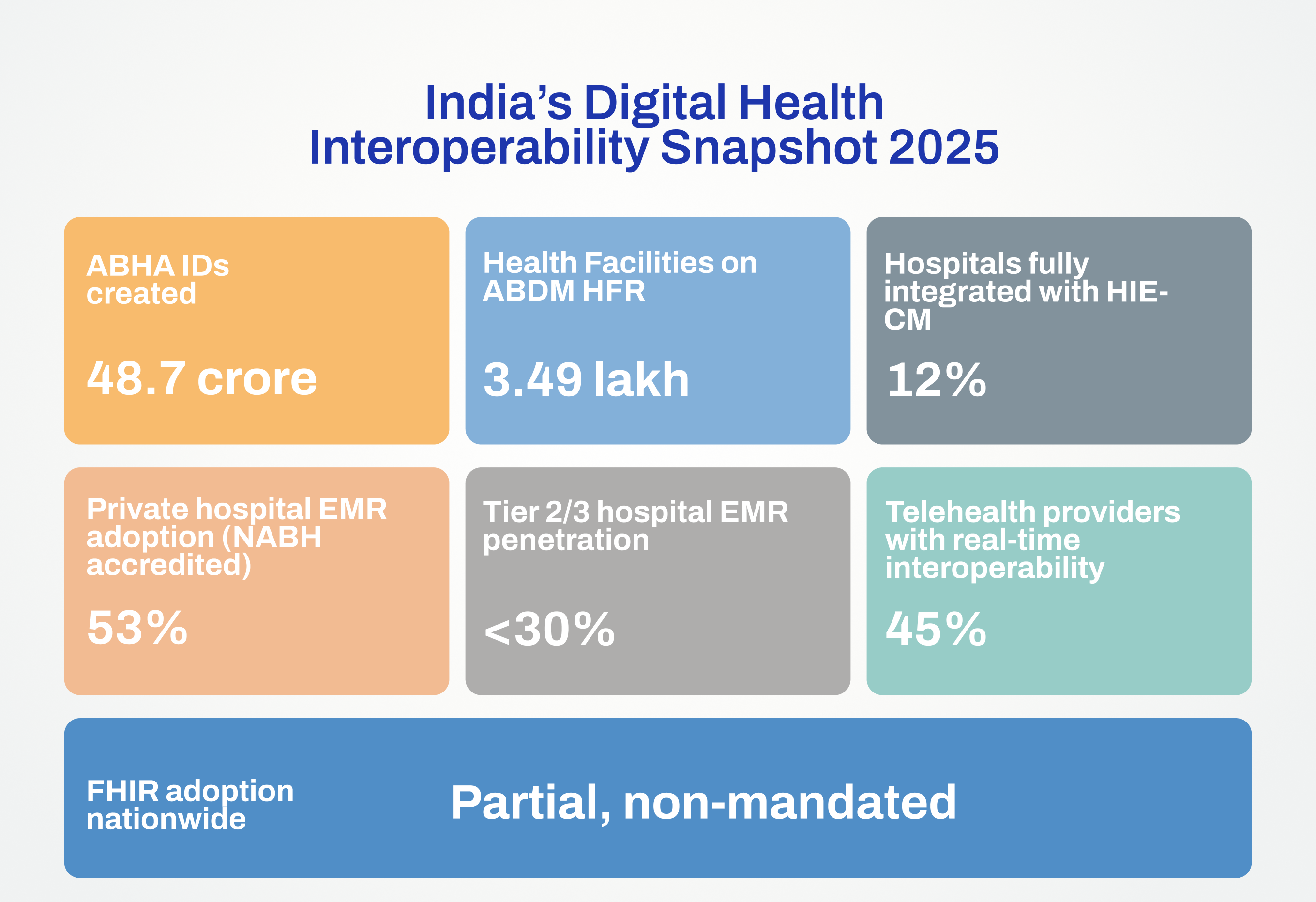
The above graphic shows - Where India Stands on Healthcare Interoperability
To unlock the full promise of digital health, India needs to move beyond siloed systems toward a truly interoperable national health infrastructure. Over the next five years, a few bold steps could accelerate this shift.
A key priority is building a secure, federated India Health Cloud, a unified data backbone connecting hospitals, labs, insurers, pharmacies, and digital health apps, while preserving data ownership at the source. Such a platform can power real-time data exchange, coordinated care, and nationwide health analytics.
The Ayushman Bharat Digital Mission (ABDM) must scale from basic record sharing to enabling full care continuum tracking and analytics. This means pushing for EMRs that are FHIR-native, enforcing interoperability standards, and ensuring all stakeholders, especially private providers are technically ready and compliant.
Integrating AI, real-time analytics, and population health tools into this ecosystem can transform early diagnosis, disease surveillance, and clinical decision-making. Unified data can help predict outbreaks, spot public health trends, and guide resource planning.
Interoperability also saves costs. Global studies estimate $30 billion in annual savings from fewer duplicate tests and medical errors. For India, the clinical and financial upside could be just as high, but it will need strong national will and coordination to realize it.
Finally, the future of interoperability in India depends on aligning policy, market incentives, and public trust. Unless hospitals, diagnostic labs, insurers, and health-tech firms see tangible value in shared health data, through operational savings, regulatory ease, or new service models, adoption will remain slow. Clear government roadmaps, predictable compliance frameworks, and visible leadership from state health authorities and private hospital networks will be crucial to sustaining momentum.
India’s healthcare system has a rare opportunity to leapfrog fragmented, closed networks and build a connected, patient-centric, data-driven digital health ecosystem from the ground up. The next three years will determine whether that opportunity is fully realized.
Disclaimer: This article is for informational purposes only. DHN does not claim ownership of the concepts, opinions, or data referenced herein. All insights are based on publicly available sources, expert commentary, and research publications.