Policy, Platforms, and People: Unpacking India’s Digital Mental Health Transition

India is standing at the cusp of a digital health revolution that could redefine how mental well-being is understood, accessed, and delivered. For decades, the country has grappled with a stark reality: mental health remained underfunded, under-discussed, and under-integrated into mainstream healthcare. But the tide is shifting.
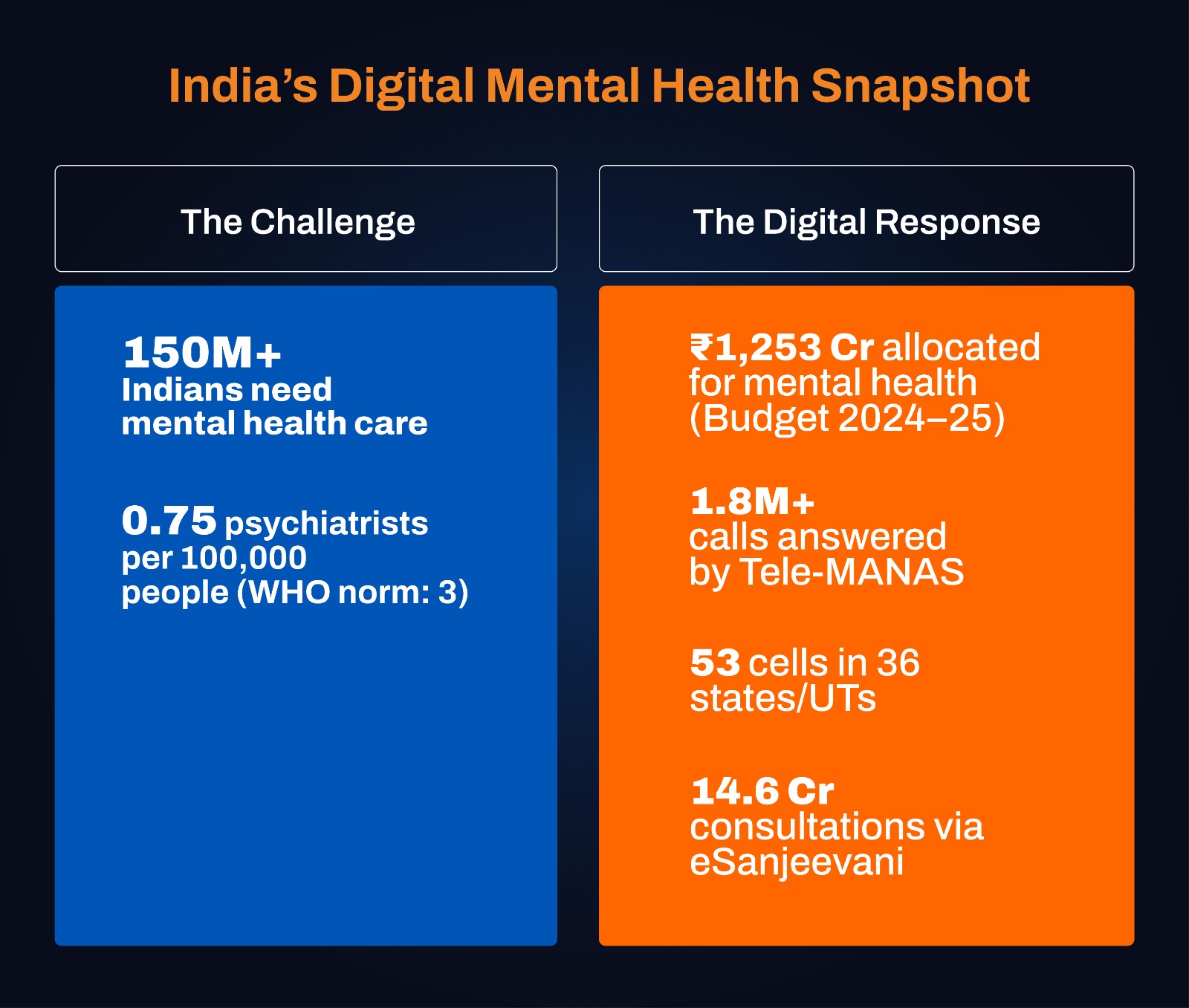
With the government investing in digital platforms such as Tele-MANAS, Ayushman Bharat Digital Mission (ABDM), and eSanjeevani, India is now attempting to bridge one of the world’s widest gaps in mental health treatment. In a country where nearly 1 in 7 people live with some form of mental disorder, technology is no longer an accessory; it is becoming the backbone of access and equity. The story is no longer just about scarcity; it is about how digital innovation can transform constraints into opportunities.
Budgetary Trends: From Symbolism to Strategy
India’s Union Budget allocations are beginning to reflect the recognition that mental health deserves. For FY 2024–25, the government allocated ₹1,614 crore for mental health programs, crossing the 1% threshold of the total health budget for the first time. Within this, NIMHANS received ₹850 crore—an 18% increase over the previous year—underscoring its role as the country’s premier training and treatment institute. Tele-MANAS was allotted ₹90 crore to scale its helpline and mobile app, while the National Mental Health Programme (NMHP) continued at ₹40 crore.
These numbers remain modest compared to the ₹36,000+ crore allocation for the National Health Mission, but the growing earmarks for digital mental health mark a clear strategic pivot. As Finance Minister Nirmala Sitharaman said in her 2022–23 Budget speech, “Mental health is critical to overall health, and digital platforms will be key in ensuring access at scale.” The challenge now is to move beyond symbolic allocations to multi-year, ring-fenced funding that guarantees sustainability.
Tele-MANAS: A Nationwide Digital Lifeline
Launched in October 2022, Tele-MANAS (Tele Mental Health Assistance and Networking Across States) has emerged as the flagship of India’s digital mental health push. By February 2025, the platform had handled 1.81 million calls, supported by 53 functional cells across 36 states and UTs, alongside 23 mentoring institutes and 5 regional coordinating centers. Its mobile app, launched in October 2024, now offers multilingual self-care modules, stress management tools, and pilot video consultations in Karnataka, Tamil Nadu, and Jammu & Kashmir. By July 2025, call volumes had crossed 2.38 million, reflecting rising awareness and trust.
Tele-MANAS is more than a helpline—it is India’s first digital entry point to structured mental health care. Backed by WHO recognition as a scalable model for LMICs, it demonstrates that with technology, India can democratize access to care for populations that were historically left out.
Anchoring Digital in Primary Care
The strength of India’s approach lies in integration. Nearly 1.77 lakh Sub Health Centres and PHCs have been transformed into Ayushman Arogya Mandirs, each mandated to provide basic mental health services. General physicians and frontline health workers at these centers are being trained—often through digital modules like iGOT-Diksha—to manage mild and moderate cases. For more complex conditions, Tele-MANAS referrals link patients to district hospitals or tertiary centers, creating a tiered care model.
This integration ensures that digital platforms are not stand-alone, but embedded within India’s broader health ecosystem, offering both scale and sustainability.
eSanjeevani & ABDM: Laying the Digital Tracks
India’s telemedicine platform, eSanjeevani, has already recorded over 14 crore consultations. Although mental health consultations are still a small share, the platform provides proof of scalability. The Ayushman Bharat Digital Mission (ABDM) strengthens this ecosystem with unique health IDs and interoperable health records, ensuring patient journeys are continuous and portable across platforms.
Imagine a patient who makes a first call on Tele-MANAS, is referred for a teleconsultation on eSanjeevani, and later follows up at an Ayushman Arogya Mandir—ABDM makes this continuity possible. For mental health, where long-term engagement is essential, this is a game-changing innovation.
The Economic Imperative: Health as Productivity
The Economic Survey 2024–25 highlighted that India’s demographic dividend will only translate into growth if the workforce is physically and mentally resilient. According to WHO, mental disorders contribute to 2,443 DALYs per 10,000 people and an age-adjusted suicide rate of 21.1 per 100,000. Between 2012 and 2030, India is projected to lose USD 1.03 trillion in economic output due to mental health conditions.
Seen this way, digital mental health is not only a public health necessity—it is an economic strategy. Investing in Tele-MANAS, ABDM, and related platforms is about safeguarding productivity, stability, and human capital.
Human Capital: Scaling Reach Through Digital Support
The National Mental Health Survey (2015–16) exposed a 70–92% treatment gap. India has just 0.75 psychiatrists per 100,000 population, far below the WHO norm of 3. Shortages extend across psychologists, psychiatric nurses, and social workers.
Digital platforms cannot replace human expertise, but they act as force multipliers. A psychiatrist in an urban hub can digitally supervise health workers across multiple districts; AI-based triaging can fast-track urgent cases; and e-learning modules can upgrade the skills of thousands of general practitioners at scale.
National Schemes: A Policy Framework for Change
Digital transformation is embedded within a broader architecture of national mental health policy:
National Mental Health Programme (NMHP) (1982): Provides community-based services, now extended to 767 districts.
Mental Healthcare Act (2017): Enshrines the right to affordable mental health care and decriminalizes suicide.
National Suicide Prevention Strategy (2022): Seeks to reduce suicide mortality by 10% by 2030.
Rights of Persons with Disabilities Act (2016): Legally recognizes mental illness as a disability, expanding rights and protections.
Together, these schemes offer a legal and institutional backbone, while digital innovations deliver reach and accessibility.
Global Lessons: Structured Scaling
Globally, blended digital models have proven most effective. The UK’s NHS Talking Therapies combine online cognitive behavioral therapy with in-person care pathways. Australia’s e-Mental Health Strategy ensures that apps and helplines are embedded within a larger clinical framework.
India’s initiatives mirror these models but need to scale faster and with greater systemic alignment. Digital pathways must always connect to physical services, preventing the risk of becoming helplines without healing.
The Road Ahead: A Triple-Engine Strategy
India’s mental health transformation requires three engines working in unison:
Enhanced Funding — Secure multi-year financing for Tele-MANAS and related platforms.
Deep Integration — Link Tele-MANAS, ABDM, and eSanjeevani into a seamless digital ecosystem.
Workforce Empowerment — Train and digitally support professionals across every district to expand reach.
With these, India can become a global leader in digital mental health innovation.
Conclusion: From Digital Promise to National Progress
India’s mental health story is shifting from neglect to innovation, from scarcity to scale. Tele-MANAS, ABDM, and eSanjeevani are no longer just platforms—they are digital lifelines for millions. They represent a philosophy that access to mental well-being should not be bound by geography, income, or stigma.
The journey ahead demands sustained investment, stronger integration, and a workforce empowered by digital tools. If these align, India will not only close its treatment gap but also set a global benchmark in how digital transformation can humanize, democratize, and revolutionize mental health care.










