Tech-Enabled Health Equity: Closing the Divide in Rural & Urban Healthcare

Healthcare in India has made huge strides, but not everyone benefits equally. While people in cities have access to world-class hospitals and technologies, those in villages still struggle to find even basic medical care. In this article, we’ll explore how technology is trying to bridge this healthcare divide between rural and urban India. From telemedicine to AI diagnostics, we’ll see where India stands, what’s working, what’s not, and what more needs to be done to make healthcare fair and accessible for all.
What is Health Equity?
Let’s begin with a question: what does it mean for a nation to be truly healthy? Is it the number of state-of-the-art hospitals it boasts? The number of medical colleges it opens every year? Or the number of doctors it produces?
The answer lies elsewhere.
A nation is truly healthy when every citizen, regardless of where they live or how much they earn, can access quality healthcare when they need it. And that’s what we call health equity.
It isn’t just about equal healthcare facilities everywhere. It’s about making sure that vulnerable and underserved communities, whether in remote villages, tribal regions, or urban slums, get the support they need to live healthier lives.
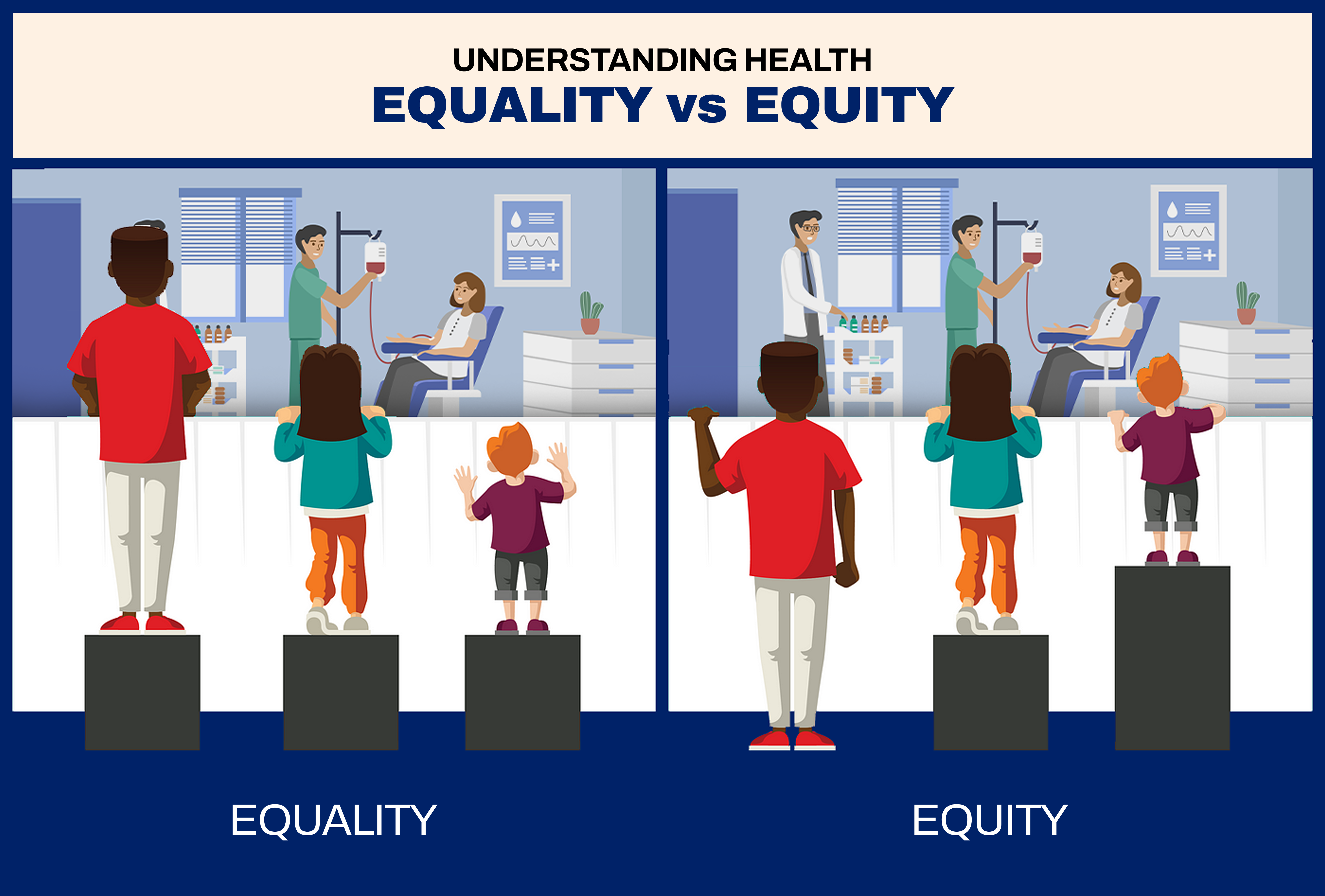
Illustration depicting the difference between Equality and Equity.
Health equity means tackling the barriers that prevent people from receiving good medical care. It means addressing poverty, illiteracy, social stigma, infrastructure gaps, and financial hardship, all of which decide whether a patient gets timely treatment or not. It’s about ensuring that healthcare isn’t a privilege for the few, but a right for all. Rather a Fundamental Right!
And where does India stand on this? That brings us to the next part.
India’s Healthtech Assessment: Where India Stands?
India is often hailed as the pharmacy of the world. We produce affordable medicines for the planet, conduct complex surgeries at a fraction of global costs, and have one of the fastest-growing healthtech markets. But scratch the surface, and a different reality emerges.
India ranks 66th out of 113 countries on the Global Health Security Index. While cities like Mumbai, Delhi, and Bengaluru boast hospitals that rival those in the West, large parts of the country remain medically underserved.
Digital health initiatives have taken off. Ever since the COVID-19 era, telemedicine services have seen a major boost in India. AI-driven diagnostics, online doctor consultations, technology is starting to bridge some of the gaps. Schemes like Ayushman Bharat Digital Mission (ABDM) aim to create a national health ID for every citizen. The private sector is innovating rapidly, and investment in healthtech startups has grown by over 45% in the last three years.
However, the benefits of these advances are largely limited to urban India.
Most rural areas lack reliable internet, smartphones, or even basic digital literacy to access these services. Telemedicine services, while promising, faces logistical hurdles, from language barriers to patchy network coverage.
Meanwhile, healthcare infrastructure in rural India still struggles with doctor shortages, outdated equipment, and crumbling facilities. Policies exist, funds are allocated, but implementation remains sluggish.
In short, India’s healthtech revolution is real but it’s unequal. And unless this gap is addressed, technology alone won’t deliver health equity.
Has Tech Improved Health Equity in India Yet?
Here’s the million-dollar question: Has technology actually made healthcare more equitable in India?
The short answer: yes, but not enough.
On one hand, India’s digital healthcare landscape has expanded faster than we imagined. Telemedicine apps, online doctor consultations, digital health records, and AI-powered diagnostic tools have made headlines and saved lives.
During the COVID-19 pandemic, teleconsultations surged by over 500%. Villages that had no doctors could suddenly speak to specialists in cities. Lives were saved, distances bridged, and technology proved its worth.
Government initiatives like the eSanjeevani platform facilitated over 20 crore teleconsultations by 2023.
Schemes like Ayushman Bharat Digital Mission aim to create a unified, tech-powered health ecosystem with digital health IDs, online prescriptions, and portable health records.
Private players too, have stepped up. Healthtech startups like Practo, 1mg, and PharmEasy are offering affordable medical services at people’s fingertips. AI is helping radiologists detect diseases faster. Drones are delivering medicines to remote regions. It’s a revolution.
But here’s the catch.
While cities enjoy these benefits, rural India is still catching up. In villages with poor internet connectivity, patchy electricity, and low digital literacy, healthtech services remain out of reach. The very people who should have benefitted most from digital healthcare have ironically been the last to access it.
A study by the Ministry of Electronics and IT in 2023 revealed that only 29% of India’s rural households have regular internet access. Telemedicine is no help when there’s no network. AI-powered diagnostics won’t work without labs and trained staff to interpret results.
So yes, technology has improved health services for millions, but its impact on true health equity is still limited. Until rural and marginalized communities can access these innovations as easily as city dwellers do, the healthcare divide will persist. And that’s the reality we need to address.
Rural vs Urban: The Persistent Healthcare Divide
Two Indias exist when it comes to medical access. One enjoys advanced hospitals, 24x7 medical care, while the other finds a clinic without a doctor, struggles to find an ambulance in emergency. Let’s break it down.
Infrastructure & Accessibility
In India’s cities, healthcare is booming. Multi-specialty hospitals, advanced diagnostic labs, and round-the-clock services are available in every metro. Private players have taken over, offering everything from heart transplants to robotic surgeries.
Now, compare that with rural India. More than 60% of our population lives in villages, but only 37% of hospital beds are available there. In many areas, people travel over 50 kilometres just to reach the nearest hospital, often in emergencies. In some districts, one ambulance serves an entire region. Let’s ask ourselves: Is it enough?
Affordability & Financial Struggles
Private hospitals charge exorbitant fees, and while government hospitals exist, they’re overcrowded and overburdened.
In rural India, people rely on government-run clinics and hospitals. But these centres are frequently short-staffed and ill-equipped. When rural patients are forced to seek treatment in cities, they bear additional travel and lodging expenses. It’s not uncommon for families to sell land or livestock to afford a hospital bill.
In 2021, out-of-pocket medical expenses in India still stood at 47.1% of total health expenditure, among the highest in the world.
Quality of Care
Urban hospitals have it all, skilled doctors, advanced technology, and faster emergency responses. Rural hospitals? They don’t.
Community Health Centers (CHCs) in villages face an 83% shortage of specialists. This includes gynaecologists, paediatricians, and cardiologists. Even basic services like X-rays or blood tests are missing from most rural clinics. Early detection of diseases like cancer or tuberculosis rarely happens, and by the time a patient reaches a hospital, it’s often too late.
Severe Doctor Shortages
Here’s a telling statistic: in urban India, there’s one doctor for every 1,500 people. In rural India, it’s one doctor for over 10,000 people.
Many government clinics, including the much-publicised Delhi’s Mohalla Clinics, remain empty. The few doctors assigned there are reluctant to stay, drawn by better salaries, safer working conditions, and career opportunities in urban hospitals.
Government schemes to send doctors to rural areas haven’t worked well. The infrastructure is poor, equipment outdated, and salaries uncompetitive.
Long Travel Distances
Emergency cases in rural areas often turn fatal because the nearest hospital is just too far away. Even when patients manage to reach a hospital, essential medicines, diagnostic machines, and trained staff are often missing. As a result, many turn to local quacks or faith healers, a dangerous gamble when lives are at stake.
High Medical Costs & Out-of-Pocket Expenses
India’s rural population continues to bear the brunt of high medical expenses. Even with schemes like Ayushman Bharat promising INR 5 lakh insurance per family, the reality is far from ideal.
Many private hospitals refuse to accept Ayushman cards, citing delays in government reimbursements. In some cases, hospitals charge patients anyway, Ayushman or not. Awareness about this scheme is another issue. Many eligible families in rural India don’t even know they can use it.
The Result: A Widening Healthcare Divide
The numbers paint a grim picture. Rural patients face poorer health outcomes, higher infant mortality rates, and lower life expectancy.
This isn’t just a medical issue. It’s an economic one.
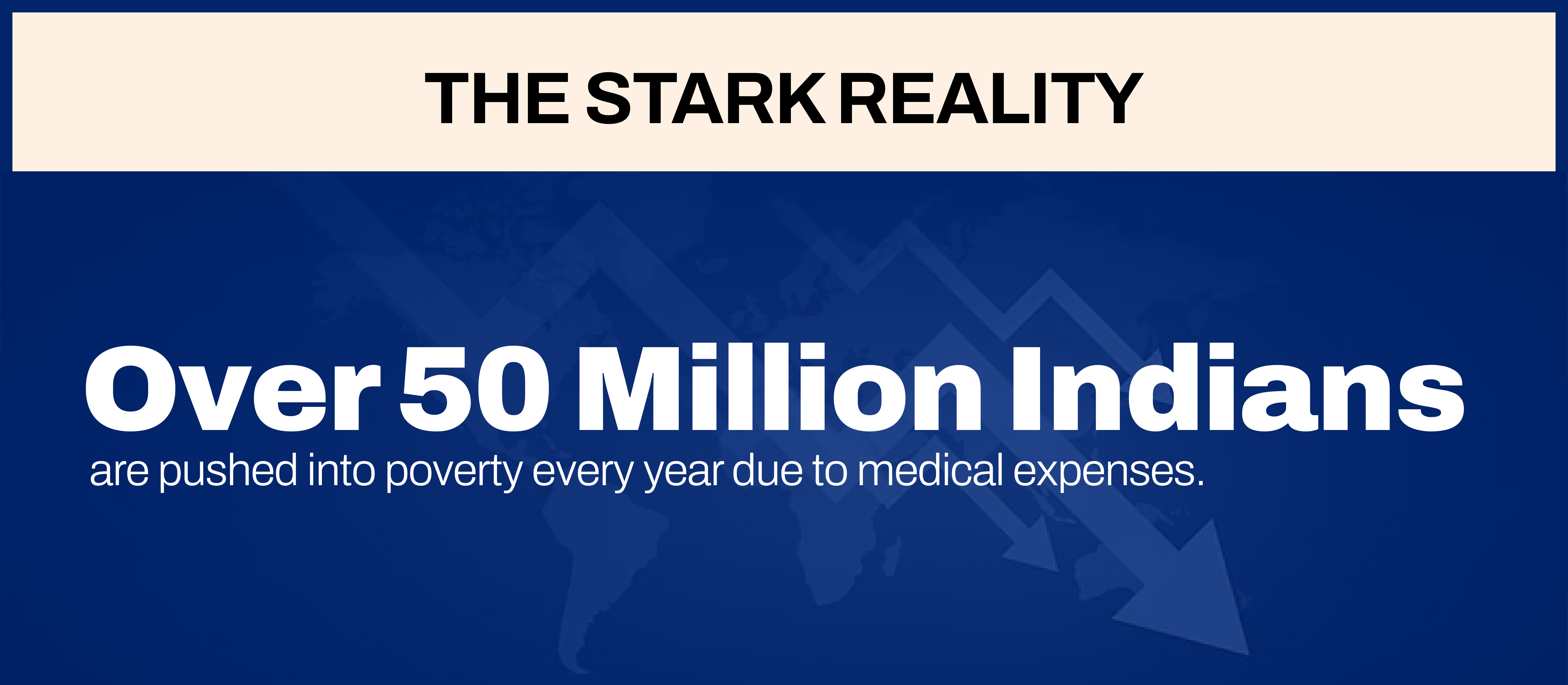
Source: WHO Report
And What’s the Solution?
It won’t be fixed overnight. Digital healthcare, AI-driven diagnostics, telemedicine, mobile health units, these are the tools India must scale up. Incentivize doctors, upgrade rural hospitals, and hold healthcare providers accountable.
Because healthcare inequality isn’t a statistic. It’s the difference between life and death.
Emerging Tech in Equalizing Access
So, we’ve established the divide. Now, let’s talk about the fix.
Is technology closing this healthcare gap? Is it reaching those remote corners of India where hospitals are scarce, and doctors are fewer? The answer is: slowly, but it’s gaining ground.
Let’s break down how.
Telemedicine & Telehealth
For millions in rural India, consulting a doctor means a long, expensive journey,sometimes over 50 kilometers, sometimes on foot, or in an overcrowded bus. Telemedicine or Video consultations are now connecting patients to doctors without either of them having to leave their spot.
E-pharmacies
E-pharmacies are delivering medicines to homes that once waited weeks for basic drugs. But there’s a flip side. The market’s still riddled with concerns of fake medicines, inconsistent regulation, and lack of awareness. If this space isn’t monitored properly, we’ll be trading one problem for another.
AI Tools
Meanwhile, AI-powered chatbots and health apps are making primary care smarter. Apps like Ada Health ask you symptom-based questions, offering advice on whether you can relax, visit a doctor, or rush to a hospital. It’s simple, effective, and in many cases, life-saving.
AI-Driven Diagnostics: In rural India, where hospitals lack labs and even basic X-ray machines, AI is stepping in as the fastest diagnostician you can imagine. Tools like Qure.ai can analyze an X-ray in seconds, flagging cases of tuberculosis, pneumonia, or even cancer.
Add predictive analytics to the mix, and healthcare systems can now identify high-risk patients before symptoms spiral out of control. And when an outbreak looms? Big data-backed disease tracking systems flag the hotspots early, giving health authorities a head start in containing infections. In places where a delay can mean disaster, this matters.
Wearables & Remote Monitoring
For chronic disease patients, those battling diabetes, heart issues, hypertension, frequent hospital visits aren’t just inconvenient; they’re risky and expensive.
Today’s smartwatches and fitness bands don’t just count steps. They track heart rates, blood pressure, oxygen levels, even detect irregular heart rhythms. Nano-based glucose monitors now help diabetics check blood sugar without painful pricks. And remote monitoring systems let doctors keep an eye on patients from miles away.
Emerging tech is rewriting the healthcare script in India. But to truly bridge the equity gap, it needs scale, regulation, and above all access. The tools exist. The challenge now is making sure they reach the people who need them most.
So, where does that leave us?
India’s healthcare story is at a critical crossroads. The technology exists. The ideas are in place. Pilot projects have shown promise. But unless these solutions move beyond metro cities and elite clinics to the country’s most remote corners, health equity will remain a dream, not a reality.
What’s Next for India’s Health Equity?
The roadmap is clear. If India truly wants to bridge the healthcare divide, three things must happen and fast.
First, rural healthcare infrastructure needs urgent investment. Telemedicine can’t function where there’s no internet. AI-driven diagnostics won’t help if basic lab equipment is missing. Without functional primary health centers, digital solutions are just digital dreams.
Second, government policies must enforce accountability. Health insurance schemes like Ayushman Bharat should be universal in both promise and practice. Hospitals denying coverage, doctors reluctant to serve villages, and scams exploiting the poor, this cannot continue.
Third, we need a cultural shift. Health literacy in rural India is still dangerously low. Superstitions, local quacks, and home remedies replace proper medical care. Technology can only work when people trust it, access it, and understand it.
Wrapping Up
At the heart of it, good health should not depend on where you live. Whether it’s a bustling metro or a small village, every person deserves timely, reliable medical care. Technology is showing us a new way forward, one where distance, cost, and infrastructure don’t decide who gets treated and who doesn’t. The journey towards health equity in India is far from over, but each digital tool, policy reform, and awareness drive brings us a little closer. It’s time to turn scattered efforts into a nationwide movement, because good health is not a privilege, it’s a basic right.